Investigation of novel SARS-CoV-2variantInvestigation of novel SARS-CoV-2variantInvestigation of novel SARS-CoV-2Investigation of novel SARS-CoV-2 Variant of Concern 202012/01 L6
Diagnostic antibodies and antigens for Companion Animal disease testing
● Rabbit
Diagnostic antibodies and antigens for Swine disease testing
Diagnostic antibodies and antigens for Avian disease testing
Diagnostic antibodies and antigens for Multiple animal disease testing
Diagnostic antibodies and antigens for Ruminant disease testing
● Deer
Diagnostic antibodies and antigens for infectious and non-infectious Equine/Horse disease testing
SOCAIL MEDIA

Technical briefing 6
This briefing provides an update on previous briefings up to 1 February 2021
Summary
There are 4 variants of concern, designated:
• VOC 202012/01 (B.1.1.7), first detected in Kent England is predominant in all regions and is circulating in multiple countries
• VOC 202102/02 (B.1.1.7 cluster with E484K mutation), first detected in South West England has been detected in 23 cases
• VOC 202012/02 (B.1.351), first detected in South Africa, 126 case have been detected in England with evidence of in country transmission. Local testing is underway and links between cases are being investigated
• VOC 202101/02 (P.1), first detected in Brazil has not been detected in the UK
Nomenclature of variants in the UK
SARS-CoV-2 variants if considered to have concerning epidemiological, immunological or pathogenic properties are raised for formal investigation. At this point they are designated Variant Under Investigation (VUI) with a year, month, and number. Following risk assessment with the relevant expert committee, they may be designated Variant of Concern (VOC).
Variant surveillance overview UK
Data on variants of concern is updated twice weekly online. Total case numbers per VOC as of 10 February 2021 are shown in Table 1.
| England genomic cases 10 February 2021 | ||||
| Variant | Pangolin lineage | confirmed | probable | total confirmed and probable |
| VOC 202012/01 | B1.1.7 | 50,148 | 5,774 | 55,922 |
| VOC 202102/02 | B.1.1.7 with E484K cluster | 23 | 0 | 23 |
| VOC 202012/02 | B.1.351 | 126 | 56 | 182 |
| VOC 202101/02 | P1 | 0 | 0 | 0 |
VOC 202012/01 (B.1.1.7)
This variant was designated VUI 202012/01 (B.1.1.7) on detection and on review re-designated as VOC 202012/01 (B.1.1.7) on 18 December 2020.
Genomic profile
Lineage defining mutations are shown in Table 2a/b. In addition, VOC 202012/01 has acquired other mutations in some cases. Mutation counts in the UK dataset are shown in Table 2c.
| S Gene | H69_V70del | 21765_21770del |
| Y144del | 21991_21993del | |
| N501Y | 23063A>T | |
| A570D | 23271C>A | |
| P681H | 23604C>A | |
| T716I | 23709C>T | |
| S982A | 24506T>G | |
| D1118H | 24914G>C | |
| ORF1ab | T1001I | 3267C>T |
| A1708D | 5388C>A | |
| I2230T | 6954T>C | |
| 3675-3677del | 11288_96del | |
| ORF8 | Q27* | 27972C>T |
| R52I | 28048G>T | |
| Y73C | 28111A>G | |
| N Gene | D3L | 28280_2delinsCTA |
| CONFIRMED | All lineage defining non-synonymous changes called as alternate base |
| PROBABLE | At least 5 lineage defining non-synonymous changes called as alternate base and all other positions either N or mixed base |
| LOW_QC | Fewer than 5 lineage defining non-synonymous changes called as alternate base and all other positions either N or mixed base |
Biological profile
VOC 202012/01 (B.1.1.7) can spread faster than some other SARS-CoV-2 virus variants currently circulating in the UK. At this time, available evidence suggests that VOC 202012/01 (B.1.1.7) is not strongly associated with antigenic escape from naturally-acquired immunity. Additionally, VOC 202012/01 (B.1.1.7) is not associated with significant antigenic escape from vaccine-acquired immunity. VOC 202012/01 (B.1.1.7) mutations do confer escape from a subset of monoclonal antibodies that target the RBD and NTD.
Transmissibility
The VOC 202012/01 (B.1.1.7) appears to have increased transmissibility compared to previously circulating variants and has spread rapidly to become the dominant variant in the UK. Previous transmissibility assessments are available in NERVTAG papers and PHE technical briefings (secondary attack rate).
Escape from natural immunity
Changes in the genome of B.1.1.7 include changes in the spike glycoprotein. Mutation N501Y can result in decreased recognition by monoclonal antibodies that bind this epitope. Deletions in the N terminal domain at residues 69/70, and particularly 144 can results in decreased monoclonal antibody binding. Since convalescent sera and vaccine-derived antisera are polyclonal, these mutations usually do not result in consequential loss of serum neutralization. These mutations could though have large effects on efficacy of monocloncal antibodies used therapeutically if they specifically target these epitopes.
Severity of disease
Summary data and analyses on severity of disease associated with B.1.1.7 are available: NERVTAG including 11 February 2021 update on severity.
Epidemiological profile
Lineage B.1.1.7 is dispersed across the UK. Confirmed cases are those identified by whole genome sequencing. As of 10 February 2021, there were 55,922 confirmed and probable cases of VOC 202012/01 (B.1.1.7) in England.
| PHE Centre | VOC 202012/01 (B.1.1.7) | All sequenced | ||
| N | % | N | % | |
| East Midlands | 1,545 | 3.1 | 6,808 | 5.2 |
| East of England | 5,934 | 11.8 | 13,445 | 10.3 |
| London | 14,672 | 29.3 | 29,350 | 22.5 |
| North East | 2,202 | 4.4 | 8,194 | 6.3 |
| North West | 10,191 | 20.3 | 28,099 | 21.5 |
| South East | 7,720 | 15.4 | 14,630 | 11.2 |
| South West | 1,468 | 2.9 | 5,126 | 3.9 |
| West Midlands | 3,587 | 7.2 | 11,300 | 8.6 |
| Yorkshire and Humber | 2,471 | 4.9 | 13,657 | 10.5 |
| TBC | 358 | 0.7 | 77 | 0.1 |
| Total | 50,148 | 130,686 | ||
S gene target failure/lineage correlation
The use of S gene target failure in the Taqpath assay as a good proxy for VOC 202012/01 (B.1.1.7) cases has been described in prior technical briefings. This continues to be supported by current data (Appendix 1). In samples tested with this assay in the Lighthouse Laboratories, samples with SGTF have predominated since mid December 2020, reaching 95.0% of cases in the week starting 7 February 2021. Proportions continue to rise by region (Appendix 1).
Hospitalisations
Assessment of hospitalisation is in process.
Deaths
1,072 deaths (within 28 days) of 50,148 confirmed cases have been reported in patients with VOC 202012/01 (B.1.1.7) as of 10 February 2021.
Cases in individuals who have been vaccinated
Assessment of vaccination data is in process.
International Epidemiology
As of the 10 February 2021 there are 90 countries/territories reporting cases of the UK variants globally. Of these, 7 report, or there is evidence of community transmission (Canada, Denmark, Ireland, Netherlands, Slovakia and USA), however for many countries the information available on the extent of transmission within the country is not always clear.
GISAID (gisaid.org) includes data on sequences available internationally; as of the 12 February 2021 6,982 cases of VOC202012/01 (B.1.1.7) other than those in the UK are listed (Argentina 1, Australia 84, Austria 233, Bangladesh 2, Belgium 579, Bosnia and Herzegovina 1, Brazil 19, Canada 61, Caribbean 3, Czech Republic 17, Democratic Republic of the Congo 2, Denmark 1,577, Ecuador 7, Finland 41, France 598, Gambia 3, Germany 92, Gibraltar 1, Greece 3, Hong Kong 4, Hungary 5, Iceland 20, India 32, Iran 1, Ireland 398, Israel 230, Italy 432, Jamaica 4, Japan 37, Jordan 42, Kuwait 1, Latvia 2, Luxembourg 32, Macedonia 2, Malaysia 2, Mayotte 18, Mexico 5, Netherlands 486, New Zealand 26, Nigeria 28, North Macedonia 3, Norway 51, Oman 1, Pakistan 2, Peru 1, Poland 10, Portugal 203, Romania 11, Singapore 45, Slovakia 69, Slovenia 1, South Africa 1, South Korea 13, Spain 468, Sri Lanka 2, St.Lucia 9, Sweden 64, Switzerland 245, Taiwan 1, Thailand 5, Trinidad and Tobago 1, Turkey 103, UAE 19, USA 522, Vietnam 1).
VOC 202102/02 (B.1.1.7 cluster with E484K)
Through routine scanning of variation in VOC 202012/01 (B.1.1.7) a small number of B.1.1.7 sequences (33 of 258504 sequences as of 11 February 2021), had acquired the spike protein mutation E484K. Information suggested more than one independent acquisition event and on investigation, this forms one predominant cluster and several separate cases or small clusters. The predominant cluster consists of 17 cases primarily in South West England, 6 elsewhere in England. This cluster was designated VUI on detection and on review re-designated as VOC 202102/02 (B.1.1.7 cluster with E484K) on 5 February 2021.
Genomic and biological profile
The cluster (VOC 202102/02 (B.1.1.7 cluster with E484K)) has the mutations previously described for VOC 202012/01 (B.1.1.7) with the addition of E484K in spike gene, L730F in orf1ab, and A173V, A398T in N gene in all cases. E484K is a mutation of concern with regards to antigenic change and receptor binding avidity, and is potentially more concerning when combined with N501Y. E484K is currently the mutation with most evidence of causing antigenic change. It arises in the presence of convalescent and vaccine-derived antisera. Several independent studies showing the impact of different antigenic variants have concluded E484K is among the single mutations with the greatest impact. Secondly, E484K is associated with increased binding to human ACE2, though it is unclear what impact this has on virus phenotype. Finally, E484K is associated with multiple variants of concern including the B.1.351 and P.1 lineages, as well as being identified as a long-term adaptation in several different immunocompromised patient studies. The other mutations specific to this cluster are not associated with any known phenotypic changes and are not present in other VOCs.
Epidemiological profile
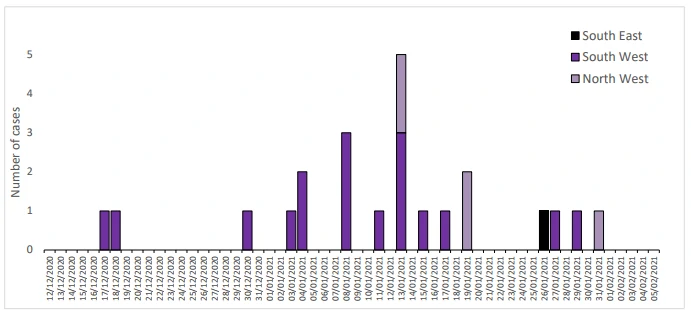
As of 11 February 2021, there were 23 genomically confirmed cases, 17 with an epidemiological link to Bristol and an additional 6 cases elsewhere in England, with a specimen date range of 17 December 2020 to 31 January 2021. The epidemiological curve for confirmed cases is shown in Figure 3. Links between cases are being investigated.
Contact tracing and control measures
Contact tracing is ongoing. Large scale testing in impacted geographies has been implemented commencing on 7 February 2021. Identification of unlinked cases through Pillar 2 is limited by sequencing coverage and time lag of at least 2 weeks between isolation and genomic confirmation. The current number of confirmed cases with this mutation may be underestimated.
Hospitalisations
Of 23 cases, data are available for 18, of which are none were hospitalised following their infection.
Deaths
Of 23 cases, data are available for 18, of which none have died.
Cases in individuals who have been vaccinated
Of 23 cases, data are available for 18, of which 1 was known to be vaccinated before the onset of infection (5 days prior).
International Epidemiology
International cases have not been reported.
VOC 202012/02 (B.1.351)
As of 10 February 2021, 126 confirmed and 56 probable cases of VOC 202012/02 (B.1.351, initially detected in South Africa) have been identified in England. This variant was designated VUI on detection and on review re-designated as VOC 202012/02 (B.1.351) on 24 December 2020.
Genomic profile
The VOC is lineage B1.351 (first sequence detected in South Africa in October 2020; and in the UK in December 2020). The complete mutation profile is shown in Table 4.
| Gene | amino_acid>T | actual_nucleotide |
| S Gene | L18F | 21614C>T |
| D80A* | 21801A>C | |
| D215G* | 22206A>G | |
| R246I | 22299G>T | |
| K417N* | 22813G>T | |
| E484K* | 23012G>A | |
| N501Y* | 23063A>T | |
| A701V* | 23664C>T | |
| 242-244del | ||
| ORF1ab | T265I | 1059C>T |
| K1655N* | 5230G>T | |
| K3353R | 10323A>G | |
| 3675-3677del | 11288_96del | |
| ORF3a | Q57H | 25563G>T |
| S171L | 25904C>T | |
| E Gene | P71L* | 26456C>T |
| N Gene | T205I* | 28887C>T |
| CONFIRMED | All lineage defining non-synonymous changes called as alternate base excluding those in red text in Table 4a |
| PROBABLE | At least 4 lineage defining non-synonymous changes called as alternate base and all other positions either N or mixed base OR at least 5 of the 9 non-synonymous changes indicated by * in the Table 4a |
| LOW_QC | Fewer than 4 lineage defining non-synonymous changes called as alternate base and all other positions either N or mixed base |
Biological profile
This variant has 9 mutations associated with transmissibility and antigenic change, of which E484K and N501Y are most significant. The significance of E484K has been described previously in this briefing. Variants with the combined N501Y and E484K substitutions have been shown to have enhanced ACE2 receptor binding.
Escape from natural immunity
Multiple studies with pseudovirus and live virus neutralization assays indicate a significant loss of antibody binding and neutralization to B.1.351, both with convalescent, as well vaccinederived polyclonal antisera.
Epidemiological profile
B1.351 is dispersed across the UK in low numbers. Confirmed cases are those identified by whole genome sequencing; probable cases are COVID-19 cases without sequencing, but who are contacts of confirmed cases. As of 10 February 2021, there are 126 confirmed cases of B.351.1 and 56 probable cases. For 18 cases, no travel link has been established indicating within country transmission. Identification of unlinked cases through Pillar 2 is limited by sequencing coverage and lag and cases are likely to be an underestimate.
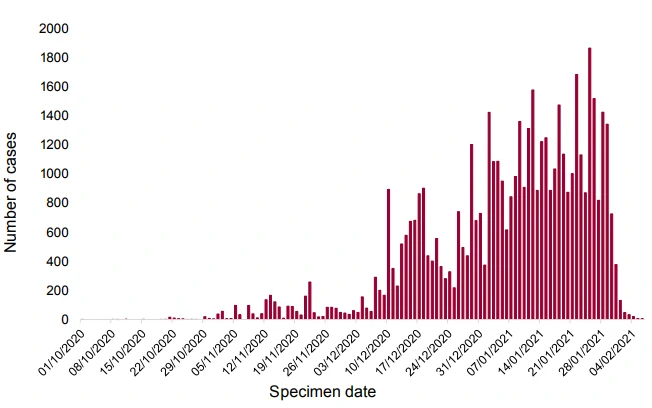
Figure 4. Epidemic curve for confirmed VOC 202012/02 (B.1.351) cases by specimen date, 10 December 2020 to 10 February 2021 (7 cases are omitted without specimen date)Percent confirmed SGTF for most recent days annotated.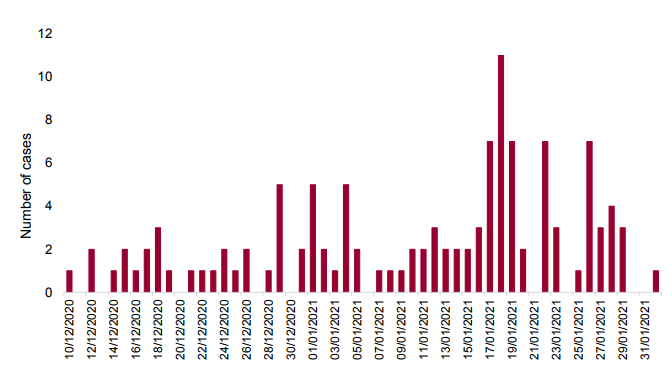
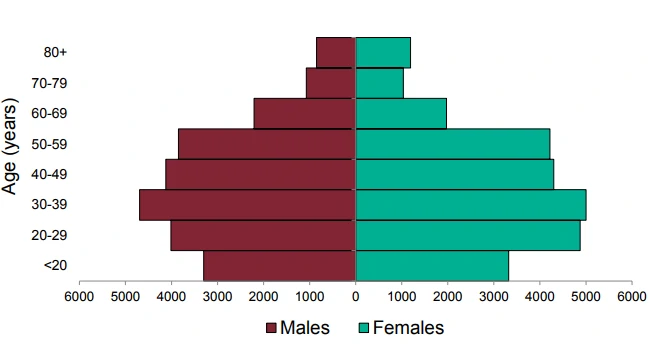
Figure 5. Age sex pyramid of VOC 202012/02 (B.1.351) confirmed cases, 10 December 2020 to 10 February 2021 (3 cases are omitted without age sex data)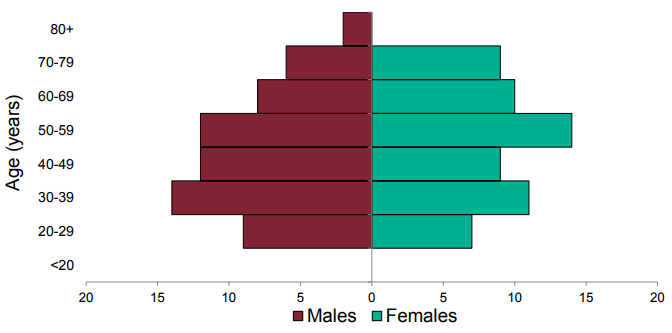
| PHE Centre | VOC 202012/02 (B.1.351) | All sequenced | ||
| n | % | n | % | |
| East Midlands | 3 | 2.4 | 6 808 | 5.2 |
| East of England | 26 | 20.6 | 13 445 | 10.3 |
| London | 31 | 24.6 | 29 350 | 22.5 |
| North East | 2 | 1.6 | 8 194 | 6.3 |
| North West | 14 | 11.1 | 28 099 | 21.5 |
| South East | 30 | 23.8 | 14 630 | 11.2 |
| South West | 4 | 3.2 | 5 126 | 3.9 |
| West Midlands | 11 | 8.7 | 11 300 | 8.6 |
| Yorkshire and Humber | 5 | 4.0 | 13 657 | 10.5 |
| TBC | 0 | 0.0 | 77 | 0.1 |
| Total | 126 | 130,686 | ||
Community prevalence studies
REACT study: Altogether 4 VOC 202012/02 (B.1.351) genomes were identified. SARS-COV-2 was detected in 2,282 of 167,642 samples during 6 to 22 January 2021. Of these, samples with CT values of 34 or less had sequencing attempted; 659 have available sequences, of which 4/659 are VOC 202012/02 (B.1.351) from East of England (2), London (1) and South East (1). All have sample dates between 7 to 11 January 2021. (Link to Study protocol.)
Office for National Statistics Survey
The ONS survey identified 2 cases of VOC 202012/02 (B.1.351) in samples from December 2020. A total of 1,816 sequences were available for 1 December 2020 to 20 January 2021.
Deaths
1 death (within 28 days) of 126 confirmed cases with data has been reported in patients with VOC 202012/02 (B.1.351) as of 10 February 2021.
Cases in individuals who have been vaccinated
Vaccination data is being assessed.
International Epidemiology
As of 10 February 2021 there are 40 countries (including the UK) that have reported cases of this variant globally.
As of 10 February 2021 the epidemiological profile in South Africa is as follows:
• The case incidence is continuing to decrease. Currently, the reported weekly incidence is 34.2 per 100,000 population. Weekly test positivity has also been decreasing with current test positivity of 9.7% (testing rates had increased over the period from around 2 per 1,000 population to over 6 per 1,000 population, although have declined slightly over the last 2 weeks to 3.5 per 1,000 population).
• The fatality rate is decreasing (the weekly fatality rate is 3.2 per 100,000 population).
• The number of patients in hospital and ICU has also reduced slightly.
Currently, 1,839 COVID-19 patients are in ICU and 11,618 are in hospital.
GISAID (gisaid.org) includes data on sequences available internationally. As of the 12 February 2021 1,130 cases of VOC 202012/02 (B.1.351) are listed (Australia 17, Austria 3, Bangladesh 1, Belgium 59, Botswana 35, Canada 1, Denmark 7, Dominican Republic of the Congo 1, Finland 2, France 39, Germany 8, Ireland 10, Israel 7, Japan 5, Kenya 6, Luxembourg 2, Mayotte 23, Mozambique 42, Netherlands 31, New Zealand 7, Norway 1, Panama 1, Portugal 1, South Africa 749, South Korea 1, Spain 2, Sweden 1, Switzerland 23, Turkey 2, UAE 5, USA 7, Zambia 31).
VOC 202101/02 (P.1)
First identified in Japan amongst travellers from Brazil, the P.1 lineage is a descendant of B.1.1.28. This variant was designated VUI on detection and on review re-designated as VOC 202101/02 (P.1) on 13 January 2021.
Genomic profile
VOC 202101/02 (P.1) is part of a larger international cluster, designated Lineage P.1 (first sequence noted in GISAID from Brazil in December 2020) and contains 17 unique amino acid changes, 3 deletions, 4 synonymous mutations, and one 4 nucleotide insertion. The complete mutation profile is shown in Table 6a.
| Gene | amino_acid>T | actual_nucleotide |
| S Gene | L18F | 21614C>T |
| T20N | 21621C>A | |
| P26S | 21638C>T | |
| D138Y | 21974G>T | |
| R190S | 22132G>T | |
| K417T | 22812A>C | |
| E484K | 23012G>A | |
| N501Y | 23063A>T | |
| H655Y | 23525C>T | |
| T1027I | 24642C>T | |
| orf1ab | – | 733T>C |
| – | 2749C>T | |
| S1188L | 3828C>T | |
| K1795Q | 5648A>C | |
| – | 11288_96del | |
| – | 12778C>T | |
| – | 13860C>T | |
| E5665D | 17259G>T | |
| orf8 | E92K | 28167G>A |
| – | 28263insAACA | |
| N Gene | P80R | 28512C>G |
| – | 28877A>T | |
| – | 28878G>C |
Red text indicates acquisition in subset of isolates within the lineage, non-variant defining mutations. Blue text indicates mutations present in the lineage but also observed in other isolates in lineage B.1.1.28, these are not included in the variant definition. Indels (shaded in orange) are not currently included in variant definitions.
| CONFIRMED | All lineage defining non-synonymous changes called as alternate base |
| PROBABLE | At least 5 lineage defining non-synonymous changes called as alternate base and all other positions either N or mixed base |
| LOW_QC | Fewer than 5 lineage defining non-synonymous changes called as alternate base and all other positions either N or mixed base |
Biological profile
This variant has mutations associated with both transmissibility and antigenic change including several in common with the B.1.351 lineage (N501Y, E484K and K417N/T). The significance of E484K has been described previously in this briefing.
Transmissibility
P.1 has been a been identified in Manaus, Brazil which experienced a rapid growth in numbers of COVID hospitalisations. Variants with the combined N501Y and E484K substitutions have been shown to have enhanced ACE2 receptor binding. Increased transmissibility is biologically and epidemiologically plausible, but at this time there is insufficient evidence to confirm or refute this. The frequency of such variants within the Brazilian population is difficult to assess.
Re-infections in healthcare workers have been reported in Brazil.
Epidemiological profile
There are no cases in the UK as of 10 February 2021
International Epidemiology
As of 10 February 2021, cases of VOC 202101/02 (P.1) have been reported in 11 countries/territories. 3 countries have reported cases of a Brazilian variant additional information is awaited to clarify if this is with VOC 202101/02 (P.1).
GISAID (gisaid.org) includes data on sequences available internationally. As of the 12 February 2021 91 cases of VOC 202101/02 (P.1) are listed (Brazil 62, Colombia 9, Faroe Islands 1, France 3, Italy 3, Japan 6, Netherlands 2, Peru 1, South Korea 1, USA 3).
Diagnostics
Lateral flow devices
Tested lateral flow devices detect VOC 202012/01 (B.1.1.7) and VOC 202012/02 (B.1.351) when assessed in a laboratory setting using variant virus materials.
Testing of VOC 202102/02 (B.1.1.7 with E484K) and VOC 202101/02 (P.1) are pending availability of virus material.
qPCR/Molecular amplification testing
A pathway is being established by MHRA to provide continued assurance of performance for diagnostic devices in use in the UK. This includes a process of analytical evaluation by PHE and NHSE, where appropriate, to formally test the impact on detection, of variants of concern, by specific products used for clinical diagnostics.
Appendices
| Week beginning | Percentage VOC of all Δ69-70 | Number of pillar 2 Δ69-70 sequences |
| 2020-10-12 | 3% | 116 |
| 2020-10-19 | 15% | 220 |
| 2020-10-26 | 29% | 156 |
| 2020-11-02 | 64% | 399 |
| 2020-11-09 | 81% | 711 |
| 2020-11-16 | 88% | 805 |
| 2020-11-23 | 93% | 390 |
| 2020-11-30 | 95% | 433 |
| 2020-12-07 | 98% | 2,712 |
| 2020-12-14 | 99% | 4,300 |
| 2020-12-21 | 99% | 2,407 |
| 2020-12-28 | 99.7% | 5,070 |
| 2021-01-04 | 99.7% | 5,621 |
| 2021-01-11 | 99.9% | 7,473 |
| 2021-01-18 | 99.8% | 6,088 |
| 2021-01-25 | 100% | 1,222 |
| Region | Percentage VOC 202012/01 (B.1.1.7) of all Δ69-70 | Number of Pillar 2 Δ69-70 1 to 31 January 2021 |
| East Midlands | 99.9% | 669 |
| East of England | 99.9% | 2095 |
| London | 99.8% | 4819 |
| North East | 100% | 871 |
| North West | 99.8% | 6615 |
| South East | 99.6% | 2875 |
| South West | 99.9% | 671 |
| West Midlands | 99.6% | 2100 |
| Yorkshire and the Humber | 99.6% | 1283 |
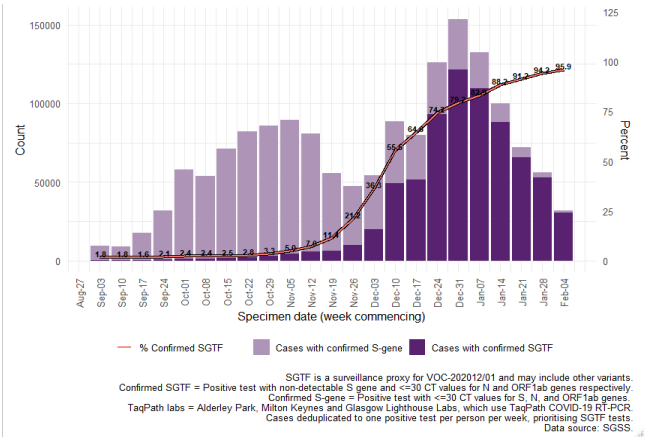 Figure 7. Weekly number and proportion of England Pillar 2 COVID-19 cases with SGTF among those tested with the TaqPath assay and with S gene detection results, by region of residence (3 September 2020 to 10 February 2021)
Figure 7. Weekly number and proportion of England Pillar 2 COVID-19 cases with SGTF among those tested with the TaqPath assay and with S gene detection results, by region of residence (3 September 2020 to 10 February 2021)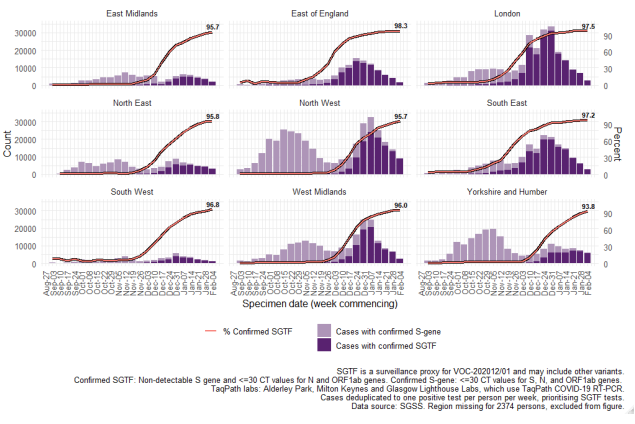 Data on coverage of TaqPath laboratories testing and numbers/proportions of cases with SGTF are shared daily with Local Authorities (Sunday to Friday) on the COVID-19 PHE Local Authorities Report Store (Sharepoint).
Data on coverage of TaqPath laboratories testing and numbers/proportions of cases with SGTF are shared daily with Local Authorities (Sunday to Friday) on the COVID-19 PHE Local Authorities Report Store (Sharepoint). Appendix 2 – Variant case definition validation
To determine if case definitions for VOC 202012/02 (B.1.351) are sufficiently sensitive, an analysis was undertaken. The current definition includes 2 different ‘probable’ definitions, outlined in Table 9. The amino acid and nucleotide substitutions characterising the variant are shown in Table 10
| Category | Definition |
| CONFIRMED | All lineage defining mutations (not in red text in Table 10) called as alternate base. |
| Probable 1 | At least 4 lineage defining mutations (not in red text in Table 10) called as alternate base and all other lineage defining positions N or mixed base. |
| Probable 2 | At least 5 of the 5 mutations (marked with * in Table 10) called as alternate base with any combination of other bases. |
| Low Quality | AFewer than 4 lineage defining mutations called as alternate base, and all other lineage defining positions N or mixed base. |
| Gene | Amino_Acid>T | Actual_Nucleotide | Note |
| S Gene | L18F | 21614C>T | not lineage defining |
| D80A* | 21801A>C | ||
| D215G* | 22206A>G | ||
| R246I | 22299G>T | not lineage defining | |
| K417N* | 22813G>T | not lineage defining | |
| E484K* | 23012G>A | ||
| N501Y* | 23063A>T | ||
| A701V* | 23664C>T | ||
| ORF1ab | T265I | 1059C>T | nsp2T85I |
| K1655N* | 5230G>T | nsp3K837N | |
| K3353R | 10323A>G | nsp5K90R | |
| ORF3a | Q57H | 25563G>T | |
| S171L | 25904C>T | ||
| E Gene | P71L* | 26456C>T | |
| N Gene | T205I* | 28887C>T |
Two data sets were included, the COG-UK genomes, and the GISAID dataset. Analysis with the COG-UK data set identified 110 confirmed UK VOC 202012/02 (B.1.351) genomes. Analysis using the GISAID data identified 463 international confirmed genomes (UK data not included). Table 11 shows the number of sequences in each category when the current probable 1 definition is used (no non-variant nucleotides NVN, sometimes referred to as wild-type, at VOC defining positions) compared to allowing one or 2 NVN calls at any of the positions.
| A Definition | Allowing 0 NVN | Allowing 1 NVN | Allowing 2 NVN |
| Both Probable | 38 | 43 | 46 |
| Probable 1 Only | 13 | 13 | 14 |
| Probably 2 Only | 8 | 3 | 0 |
| Total Probable | 59 | 59 | 60 |
| B Definition | Allowing 0 NVN | Allowing 1 NVN | Allowing 2 NVN |
| Both Probable | 96 | 259 | 278 |
| Probable 1 Only | 5 | 5 | 5 |
| Probably 2 Only | 190 | 27 | 8 |
| Total Probable | 291 | 291 | 291 |
Spike drop out and mutations or bases of poor quality data impact variant assignment using both probable 1 and 2 definitions. Analysis shows probable 1 definition detects sequences that the probable 2 definition does not, because of uncalled nucleotides in the genomes. Probable 1 definition enables variant assignment of lower QC VOC 202012/02 (B.1.351) sequences. Conversly, there are genomes that are detected using the probable 2 definition only, potentially due to reversions at some of the lineage defining positions. Currently the low-quality definition does not allow for NVN calls and therefore will not detect genomes that include data omissions, and partially meet the probable 2 definition. Therefore both definitions must be used for variant assignment. Low quality genomes currently undergo a manual review to determine whether they are considered likely to be VOC 202012/02 (B.1.351) genomes and public health action is required. Therefore, it is recommended that the low-quality definition is expanded to capture these genomes. Both probable definition 1 and definition 2 must continue to be used to enable maximum assignment of variants in addition to manual check of low-quality sequences.
Data sources
Data used in this investigation is derived from the COG-UK dataset, the PHE Second Generation Surveillance System, NHS Test and Trace, the secondary uses service (SUS) dataset and Emergency Care Data Set (ECDS).
Variant Technical Group
Organisations
This group includes representation from the following organisations: PHE, DHSC, BEIS, Wales NHS, PHScotland, NHS Scotland, Health and Social Care Northern Ireland, Imperial College London, London School of Hygiene and Tropical Medicine, University of Birmingham, University of Cambridge, University of Edinburgh, University of Liverpool, the Wellcome Sanger Institute.
Additional contributions
Additional contributions were received from REACT-1 study (Steven Riley, Oliver Eales and Paul Elliott on behalf of the REACT Study Investigators, Imperial College London).
Acknowledgements
The authors are grateful to those teams and groups providing data for this analysis, including: the Lighthouse Laboratories, COG-UK, the Wellcome Sanger Institute, the PHE Epidemiology Cell, Contact Tracing, Genomics and Outbreak Surveillance Teams.
Published February 2021
PHE gateway number: GW-1934